Recognizing Undiagnosed Adult ADHD in Clinical Practice: A Clinician's Guide
- Cody Thomas Rounds

- Aug 8, 2025
- 7 min read
Five Key Takeaways for Clinicians:
Listen to the Life Narrative: Undiagnosed ADHD in adults is a story of chronic struggle, not just a list of present symptoms.
Recognize Masking: Many adults with ADHD develop sophisticated coping mechanisms that hide the core disorder, leading to secondary symptoms like anxiety or burnout.
Differentiate Carefully: The symptoms of ADHD frequently overlap with anxiety, depression, and PTSD; the key is to look at the source and history of the symptoms.
Watch for Executive Dysfunction: This is the most consistent and telling sign, often manifesting as a lifetime of poor time management, disorganization, and overwhelm.
Refer for Formal Testing: When clinical suspicion is high based on a patient's history and screening tools, a referral to a specialist is the most responsible next step for accurate diagnosis and treatment.
Attention-Deficit/Hyperactivity Disorder (ADHD) has historically been understood as a childhood condition, often mislabeled as a phase that people simply outgrow. This outdated view has contributed to a significant population of adults who remain undiagnosed, silently struggling with the persistent symptoms of a neurodevelopmental disorder. For the clinician in private practice, these individuals rarely present with a direct concern about ADHD. Instead, they arrive with a history of secondary, often comorbid, conditions such as chronic anxiety, depression, professional burnout, or interpersonal conflict.
The most potent tool in your diagnostic arsenal is not a symptom checklist, but the patient's narrative itself. By compassionately exploring their life story—the "echoes of their past"—you can identify a consistent, though often masked, thread of ADHD woven throughout their experience. This article provides a clinical framework for recognizing these key indicators, distinguishing ADHD from similar conditions, and confidently determining when a referral for a formal assessment is the appropriate next step.
Unlocking the Patient’s Story: Using Past Narratives to Identify Adult ADHD
When an adult patient discusses their life history, listen for a recurring narrative of struggle and perceived failure despite evident intelligence. They may describe a pattern of starting jobs with great enthusiasm only to leave due to boredom or disorganization, a trail of forgotten appointments, or a feeling of being a "late bloomer" who never quite lived up to their potential. These disclosures are often accompanied by a profound sense of shame, guilt, or feeling fundamentally "lazy." They are not just anecdotal details; they are critical diagnostic data points.
Probing into their academic history can be particularly revealing. Did teachers frequently say they were "smart but could do better?" Did they struggle with completing assignments, losing materials, or sitting still in class, even if they performed well in subjects they found engaging? Ask about their relationship with time, which for an individual with ADHD, is often a source of perpetual conflict. They may have a lifelong history of being late, missing deadlines, and chronically underestimating the time required for tasks. It is crucial to remember that the absence of a formal ADHD diagnosis in childhood is not an exclusionary criterion; it is often part of the story, as their symptoms may have been misattributed to personality traits or simply overlooked.
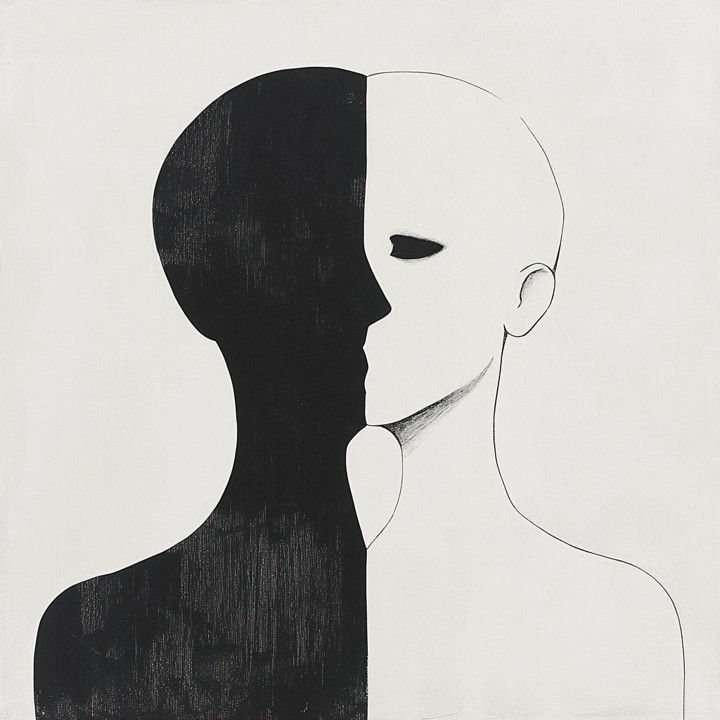
Why Adult ADHD Symptoms are Often Masked: The Art of Compensatory Behaviors
The classic stereotype of a hyperactive young boy makes it difficult to recognize ADHD in adults, particularly in women or those with the inattentive presentation. Over a lifetime, these individuals have developed sophisticated, often exhausting, coping mechanisms to navigate a world built for neurotypical brains. This "masking" can effectively hide the core disorder.
Consider hyperfocus, a common but misunderstood symptom of ADHD, which can be mistaken for high-level functioning. An adult may excel in a fast-paced, high-stakes career, but at what cost? This success often comes at the expense of their personal life, health, and relationships, as they live in a constant state of "all or nothing." A patient might have developed rigid routines and meticulous systems to compensate for poor executive function, appearing highly organized. Yet, any disruption to this fragile system can lead to catastrophic overwhelm and an inability to function. Another patient might present as a people-pleaser, meticulously remembering details about others to build a reputation for reliability, all while their own home and personal life are in disarray. These adaptive strategies are often effective enough to prevent an official diagnosis, but they are not sustainable. The constant effort required to maintain them often results in the very secondary symptoms (burnout, anxiety, depression) that bring the patient to your office.
ADHD vs. Anxiety, Depression, and PTSD: Differentiating Similar Clinical Conditions
The significant overlap in symptoms between ADHD and other common conditions necessitates careful and thoughtful differential diagnosis. A superficial assessment can easily lead to a misdiagnosis of anxiety, depression, or a personality disorder.
ADHD vs. Anxiety Disorders: Both can involve restlessness, irritability, and a feeling of being overwhelmed. The key differentiator is the source of the anxiety. In Generalized Anxiety Disorder (GAD), the anxiety is typically focused on a wide range of future events or a persistent sense of worry. In ADHD, anxiety is often a reaction to the chaos caused by ADHD symptoms: the fear of being late, forgetting a crucial task, or being judged for a mistake. The anxiety is reactive and situational, a direct consequence of executive dysfunction.
ADHD vs. Mood Disorders (Bipolar Disorder): A patient with ADHD can exhibit emotional dysregulation that might be confused with the "ups and downs" of Bipolar Disorder. The critical difference lies in the duration and nature of the mood states. Bipolar episodes are typically sustained, lasting for days or weeks, and represent a fundamental shift in mood. In contrast, the rapid mood swings in ADHD are often brief, triggered by an immediate event (e.g., frustration, boredom, or perceived rejection), and are better characterized as emotional dysregulation rather than a true mood state.
ADHD vs. Trauma (PTSD): The hypervigilance, difficulty concentrating, and emotional reactivity of PTSD can closely mimic ADHD. The patient's history is the key distinguishing factor. A person with PTSD will have a clear traumatic event or series of events that can be directly linked to the onset of their symptoms. While a person with ADHD may have a history of trauma, the core symptoms of inattention and hyperactivity/impulsivity typically predate the trauma and have been present since childhood. In many cases, the two conditions can be comorbid, complicating the clinical picture.
ADHD vs. Autism Spectrum Disorder (ASD): Both are neurodevelopmental disorders that can involve difficulties with social communication and executive function. However, the underlying drivers are different. An individual with ASD may struggle socially due to difficulties with understanding social cues, while a person with ADHD may struggle due to impulsivity, interrupting others, or inattention during conversations. The intense focus seen in ASD is typically a narrow, specific interest, whereas ADHD hyperfocus is more variable and tied to the novelty or intrinsic interest of a task.
Five Critical Indicators of Undiagnosed Adult ADHD for Clinicians
Beyond the patient’s narrative, here are five practical signs that should raise your clinical suspicion of adult ADHD:
Chronic Executive Dysfunction: This is the most consistent and telling sign. The patient describes a lifetime struggle with time management, organization, planning, and prioritization. They may feel chronically overwhelmed by tasks others find simple, their home or office may be chronically cluttered, and they may have a history of losing personal items frequently.
Emotional Dysregulation: Look for a low frustration tolerance, impatience, quick temper, and a tendency to take things personally. This often presents as Rejection Sensitive Dysphoria (RSD), an intense emotional pain response to perceived criticism or rejection, which can lead to significant interpersonal conflict and social withdrawal.
Inner Restlessness (Not Just Hyperactivity): The physical hyperactivity of childhood often transforms into a persistent inner restlessness in adulthood. The patient may describe feeling fidgety, unable to relax, or having a constant need to be doing something. They might pace during phone calls, doodle in meetings, or find themselves unable to sit through a movie without feeling a need to move.
A History of Highs and Lows: This is not Bipolar Disorder, but a pattern of starting projects or hobbies with extreme enthusiasm and then abandoning them when the novelty wears off. The patient may have a long list of unfinished degrees, projects, or business ideas. This is a tell-tale sign of a brain driven by novelty and stimulation.
Perceived Underachievement: This is a core component for many and a powerful driver for seeking help. They may have a deep-seated sense of not living up to their potential, despite being intelligent and capable. This leads to a feeling of inadequacy that is often at the root of their presenting symptoms.
Navigating the Referral Process: When to Seek Formal Adult ADHD Testing
Your role as a clinician is to identify the signs that warrant further investigation, not to make a definitive diagnosis in a single session. A referral is a critical and responsible step that is indicated when:
Clinical suspicion is high based on a consistent, longitudinal history that includes multiple indicators described above. Your initial impression suggests that executive dysfunction and inattention have been a lifelong pattern, not a recent development.
The patient's current symptoms are not fully explained by other conditions. If a solid diagnosis of GAD has been made, but the anxiety persists despite appropriate treatment, and the patient's narrative points to a history of ADHD-like struggles, it may be time to consider the underlying condition.
Standardized screening tools suggest a high probability. Utilizing an adult ADHD rating scale (such as the ASRS-V1.1) in your practice can be a helpful screening tool. A high score on such a scale, combined with a compelling history, is a strong signal for a referral.
The patient's life is significantly impacted across multiple domains. When a patient's work, relationships, finances, and emotional well-being are all consistently suffering due to issues with organization, time, and emotional control, a formal diagnosis is warranted to provide the proper treatment pathway.
By referring to a specialist who can conduct a comprehensive diagnostic evaluation, you are ensuring the patient receives the most accurate and effective care. This opens the door to treatments—including medication and therapeutic interventions—that can profoundly improve their quality of life.
Conclusion
The recognition of adult ADHD is a journey that begins with a shift in perspective. It requires us to look beyond the presenting symptoms and to listen, truly listen, to the patient’s life story. By understanding the intricate ways in which ADHD can be masked and by carefully differentiating it from other conditions, we can become more effective and compassionate clinicians. Acknowledging that the chronic struggles described by a patient may have a neurodevelopmental root not only validates their experience but also opens the door to a path of self-understanding and effective treatment that they may never have thought possible. By paying attention to these key indicators and knowing when to refer, you are not just treating symptoms; you are changing a life.
Additional Resources for Clinicians
Whether you're navigating your first years in private practice or refining your approach as a seasoned professional, PsychAtWork Pro offers tools designed with real clinicians in mind. From reflective journal series and practice-building guides to advocacy insights and supervision supports, these resources aim to deepen your practice—not just expand your toolbox.
Clinician Services
Supervision, consultation, and collaborative assessment or clinicians navigating complex cases. From licensure supervision to targeted training in assessment, diagnosis, and therapeutic modalities, these services offer reflective, rigorous support to deepen skill, sharpen insight, and move clinical work forward.









